Why do people with epilepsy respond to different medications while others are unable to find a medication that controls their seizures? It’s a fascinating question and the answer lies in a combination of three variables:
- i) there are many different forms of epilepsy
- ii) there are many different causes of epilepsy, and as a consequence
- iii) each medication is tailored to a different therapeutic mechanism
In this article I provide a discussion, in lay terms, of how medications control seizures by making analogies between a mechanic’s toolkit and a neurologist’s medicines, then go on to discuss how currently prescribed treatments change the brain to prevent seizures. My goal is to use the combination of my personal journey with epilepsy together with my neuroscience expertise, and ability to speak to the lay audience, to communicate complex processes. I hope this helps you understand epilepsy and its treatment. Please leave questions in the comment section.
Advances in Epilepsy Treatment
Epilepsy was first documented earlier than 600 B.C. on a Babylonian tablet that is currently located in the British museum. The medical community and biopharma have made significant advancements in treatment options since that time period that are still in use today, including early diet-based interventions, such as the ketogenic diet. Then, beginning in the early 1900s, novel medications were developed. Starting with phenobarbital in 1912, several additional medications were developed throughout the 20th century and into the early 2000s. For 60%-70% of people, a single or combination of medications, at the right dose(s), will prevent further seizures. In many cases, with little if any side-effects. But for 30-40% of people, medications don’t work. Some people search for years, with the assistance of their medical team, for an effective medication to control their seizures. In doing so, they go through months or even years of personal experimentation, testing different medicines at different doses until they find a medicine that works, and with acceptable side-effects. One individual may be effectively controlled by one medication, but another person may have to try several medications, and doses, before a drug is found to be effective. Unfortunately for some, an effective drug-based treatment is never found.
It has been known for centuries that there are many forms of epilepsy. As a result, we talk about the epilepsies, each of which can have a unique presentation, e.g. generalized versus focal seizures, tonic-clonic seizures, absence seizures, juvenile myoclonic seizures and the list goes on and on. But why doesn’t a medicine work for all of these epilepsies? Epilepsy can be the result of a variety of causes, including head injury, stroke, genetic factors (and there are many distinct genetic factors), developmental disorders, brain tumors as well as other unidentified causes. Consequently, different medicines are needed in the neurologist’s toolbox to treat the different types of epilepsy.
Finding The Right Tool for the Job

To develop a medicine one first needs an understanding of the biological process, why it has stopped working correctly, and then develop a solution to correct the error.
Think of the body like a car. The engine, or brain, is necessary to propel the car down the road. There are many reasons that an engine won’t start or if it does start, the car still won’t function normally. A lack of fuel, a lack of air supply needed for combustion, an electrical fault that prevents a spark, a dead battery, or perhaps some external force has caused damage. To fix the car, it is necessary first to diagnose the cause of the problem, then determine the appropriate tool to fix it and get the car running again.
Fixing the brain is a similar process: identify the cause of the problem, then choose the tool (medicine) to treat the issue. But a major difference is we built the car. We know its every component and how it works – there is even a manual. By contrast, we didn’t build the brain and we know so little about how it works. Consequently, we don’t always have the tools available to fix it when it works incorrectly. Now, think of the epilepsies like the different manifestations of engine failure in a car, all caused by different components of the car not behaving correctly. It becomes clear why one medication won’t fix all types of epilepsy; perhaps the tool or drug pulled from the toolbox is the equivalent to replacing a faulty battery. But a new battery won’t fix an empty coolant tank.
The Frustration/Uncertainty of Trial and Error in Controlling Seizures
Given that there are a variety of causes, as well as different forms of epilepsy that may arise from different brain regions and through different mechanisms, it is not surprising that it becomes necessary to perform a personalized search to find a medication that is effective. Let’s try a new battery. No, that didn’t work. What about adding more coolant? Yes, success. But how much coolant to add? There is no line to show max fill, causing an overflow. Now, we have to experiment with quantity, to get just the right amount. For the person with epilepsy, this can be a frustrating time in their life. As they try a different medicine, they don’t know whether it will work for them. Also, a dosage may be found that controls the seizures but causes such debilitating side effects that the use of the medicine cannot be tolerated.
From my own personal experience, it is frustrating not to know if the next drug will work or if the dosage of the drug will be correct. It becomes easy to believe that no effective medicine will be found. It took four years to get me medicated without serious side-effects. Initially I was taking one of the earliest anti-convulsants that had been developed, phenobarbital. However, this drug is also used to treat sleep disorders. Consequently, I kept falling asleep while at school. I was taken off this drug and prescribed Valproate and Phenytoin. Seizures were eventually controlled.

Prior to attending Leeds University, I was taken off all of my medications over a few weeks (not a current practice) and on my first day at University I had seizures: that certainly made me a notable figure with my new college mates. Subsequently, I was back on Valproate and Phenytoin and I have been seizure free for over 40 years. In 2011 I developed a life-threatening inflammatory reaction to Phenytoin. I felt like I was starting all over again as I now needed to try a new medicine. I was so anxious, would this new tool work and do so without side-effects? Phenytoin was switched to Keppra (Levetiracetam). Every day for the first few months I wondered “Will I have a seizure today?” You start to look at your future life wondering what form it will take. I am fortunate to be controlled by medications, but a week does not go by when I wonder, will I have another seizure?
How Do Anti-Epileptic Drugs Change the Brain?
So, how do medicines actually prevent seizures? Put another way, what is their mechanism of action or how does the medicine modify the brain to prevent seizures?
In the pharmaceutical industry a medicine is intended to change the activity of a specific biological target. Continuing with mechanical analogies, this is like matching the right sized wrench (drug) to tighten a nut (the target). How do some of the medicines work that control seizures? Beneath we list some common anti-epileptic drugs (AEDs) together with their target or mechanism of action. To develop these treatments, we first had to better understand how the brain worked.

One way of viewing the brain is in terms of its overall excitability or level of electrical activity. The brain is made up of billions of nerve cells, also known as neurons. Each neuron is a building block of the brain that consists of an input end and an output end. A cable stretches between the input and output, along which electrical impulses travel. When the electrical impulse reaches the output end, it stimulates the release of a chemical transmitter, which then communicates with the “input” end of another neuron (see figure above). This release of chemical transmitter (yellow packages) occurs at a structure called the chemical synapse (gap), during a process called synaptic transmission. AEDs broadly work by affecting either i) the electrical impulse, or ii) synaptic transmission.
Some AEDs (e.g Phenytoin and Lamotrigine) inhibit the sodium and calcium channels that generate the electrical impulses passing from neuron to neuron, thereby reducing the overall electrical excitability.
Some common Anti-Epilpesy Drugs (AEDs), when they were developed, how they work and their main use.
| AED | Year of approval | Presumed main mechanisms of action | Main Utility |
|---|---|---|---|
| Phenobarbital | 1912 | GABA potentiation (increase inhibition) | Broad use for focal and generalized seizures |
| Phenytoin | 1938 | Sodium channel blocker (Reduce electrical activity) | First-line AED |
| Diazepam | 1963 | GABA potentiation (increase inhibition) | Broad use for focal and generalized seizures |
| Valproate | 1967 | Multiple (for example, GABA potentiation (increase inhibition), glutamate inhibition (reduce excitation), sodium channel and T-type calcium channel blockade) | Broad use for focal and generalized seizures, first-line AED |
| Lamotrigine | 1990 | Sodium channel blocker (Reduce electrical activity) | Broad use for focal and generalized seizures, first-line AED |
| Topiramate | 1995 | Multiple (GABA potentiation, glutamate inhibition, sodium and calcium channel blockade) | Broad use for focal and generalized seizures, first-line AED |
| Levetiracetam | 2000 | SV2A modulation | First-line AED |
| Stiripentol | 2002 | GABA potentiation, sodium channel blocker |
Other AEDs act by changing the strength of the chemical signal that transmits at the synapse. Some chemical transmitters stimulate (excite) and others inhibit neuronal activity. This is much like the gas and brake pedals of a car. Just like driving a car requires the correct balance of depressing the gas and brake pedals, correct brain function requires the correct balance of inhibition and excitation.
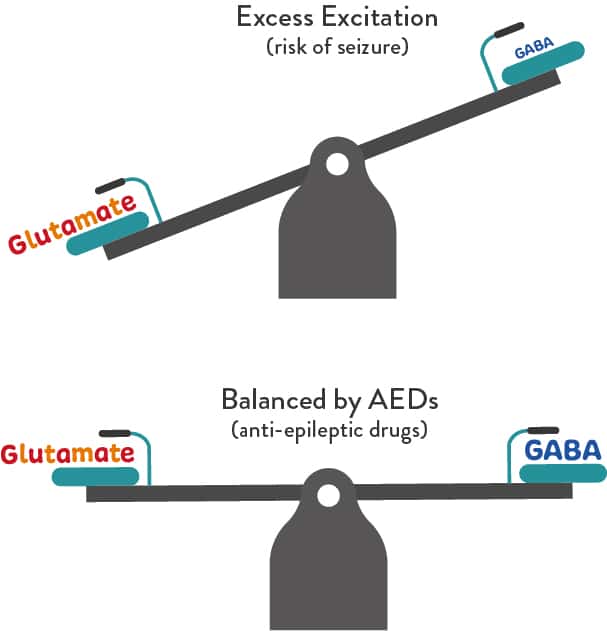
There are two major types of chemical or neurotransmitters released during synaptic transmission. One is inhibitory and is called gamma amino butyric acid (GABA). The other is excitatory and is called glutamate. These two transmitters act in tandem to control the overall electrical excitability of the nervous system highway.
If there is too much excitability in the nervous system, seizures can result. To reduce the speed of the car (or excitability of the nervous system) one could increase the pressure to the brake pedal (increase GABA inhibitory transmitter) or reduce the pressure applied to the gas pedal (reduce glutamate excitatory transmitter).
The goal of most of the effective medicines available today is to reduce the overall electrical excitability of the nervous system and reduce the probability of a seizure. Many drugs target the GABA transmitter system to increase inhibition (which is achieved by Phenobarbital, Valproate and Stiripentol), Other drugs target the glutamate system to reduce excitation (e.g. which is achieved by Topirimate and Valproate) which reduces the overall excitability.
Continued Research is Essential to Add More Tools to the Kit
Given the variety of causes and types of seizures it is not surprising that 30-40% of people with the epilepsies are not medically controlled. We have learned a lot about how the brain works but there are some parts of the brain that we don’t understand well enough yet. Until we do, we won’t be able to fix the brain when there is a problem.
It is therefore essential that we fund more research to find the underlying causes of such uncontrolled epilepsies and develop new therapies. When I became Chair of Neuroscience at Tufts University School of Medicine, one of my goals was to hire researchers who study epilepsy. Now in Sail For Epilepsy, one of our goals is to raise funds to support research into the causes of epilepsy. A portion of all funds donated to Sail For Epilepsy immediately go to fund research into identifying causes of epilepsy and into finding cures for epilepsy.
If you’d like to help, please donate here.

A very good explanatory article