@ 12:00 GMT
Position: 27° 40′ 48.4602″ N x 78° 46′ 34.626″ W
Course: 67° True
Speed: 6 kts
Blog written by crew member Greg Martin
During the past 30 years designing medical devices, I have been involved in a number of studies to test them in the laboratory and also in the clinic. I never thought that my professional vocation would intersect with my love of sailing. Yet recently, my wife (also an avid sailor) and I volunteered to be part of a 5-person crew to sail a 50-foot catamaran across the North Atlantic from Florida to the Azores.
So, what do you do when you have a crew that includes scientists and an engineer, 4 of us with PhD’s? You design a clinical study. During this 21 day or so passage, we will need to keep a continual watch. This is common among sailing vessels to keep an eye on the sails, the wind and the horizon for other vessels. Our watch schedule will probably be something like each person serves 4 hours on and then gets 6 hours off in which to sleep, which means that each crew member will have a rotating sleep schedule. Of course, we all know in advance that not getting enough sleep for 3 weeks may impact our physical and mental performance as sailors. One way to leverage this experience is perform our own onboard clinical study to better understand these effects.
This will be a modest pilot study with a maximum of 5 participants for our Florida to Azores crossing, however we still would like to abide by human subjects guidelines and be able to publish the results. So we reached out to the amazing folks at WCG IRB (https://www.wcgirb.com/) who provided the internal review board approval of our observational protocol.
As far as the elements of the protocol, we aimed to keep them very simple – an objective vigilance assessment, a sleep diary, and some form of sleep state measurement.
There already exists psychomotor vigilance tests that assess a person’s reaction rate, which can deteriorate with lack of sleep. In fact, there are free cell phone apps expressly for this purpose that we can easily adopt as part of our study. To qualitatively assess quality of sleep, our study participants (i.e., the entire crew) will keep sleep journals to note the time and duration of sleep, any relevant food or medications (including coffee and sea-sickness drugs) and how they generally feel when they are awake.
To quantitatively assess sleep, we could use a FitBit, Apple watch or some other wearable fitness device. However, almost all of these devices use their internal accelerometers to assess a person’s movement and use these data to determine if a person is awake or having restless sleep. We would expect the motion of the boat to confound these measurements. An independent accelerometer for the boat (a BoatBit?) might measure the background motion, but we would have no way to subtract this from the subject’s acceleration, then feed these data back into the wearable’s sleep algorithm – which is somewhat of a proprietary black box.
In a sleep clinical, an onshore sleep study would measure a subject’s motion, heart rate, blood oxygenation, eye movement and electroencephalogram (EEG). In addition, the subject would be video recorded during their sleep. A trained sleep technician would then take all these data and make a determination of the sleep stage (REM, non-REM, and the various non-REM sleep stages) throughout their rest. On board, we really don’t have access to this roomful of equipment (nor do with have the space). And while we don’t have a sleep technician, our skipper and Sail For Epilepsy’s president is an expert on sleep.
The most we could do for quantitative sleep assessment is to see if we can measure EEGs while at sea. And lo and behold, there are a number of companies out there that market mobile, battery-powered EEG devices. In general, EEG devices connect electrodes to a person’s scalp to record electrical signals emanating from different parts of the brain. The waveforms can indicate if a person is awake or asleep and, if asleep, the depth to which they are unconscious. However, by the time (or distance) that these signals travel from the brain to the scalp, the electrical signals are reduced to millionths of volts. So, a good electrical connection to the scalp and an amplifier are necessary. The best electrical connections are made with “wet” electrodes that contain tiny sponges to use the electrical conductivity of salt water (or saline) to help bridge the connection to the scalp. Certainly, we will have access to plenty of salt water. Dry electrodes also exist, but more pressure is required to push these electrodes onto the scalp and improve the electrical connection. In some cases, this pressure can be uncomfortable, especially if you are trying to sleep.

In finding an optimal EEG system, we considered 8 commercially available devices, some with FDA clearance, some with European approval and others consumer products intended for home use. Our main initial requirement was to identify a system that could record using battery power for at least 5 hours, be wearable during sleep (on a sailboat), not require a connection to the internet and be affordable to a non-profit organization. Most companies we spoke with were very enthusiastic about our mission. ANT-Neuro was kind enough to send us a system for evaluation purposes. This product has over 24 wet electrodes mounted on a hair-net like cap for easy deployment and it is currently being used on the International Space Station. In the end, we decided that this device was too complex for usage in our modest oceanic station.

The consumer devices considered were the Dreem and the BrainBit, both use dry electrodes. In our conversations with the Division of Sleep Medicine at Harvard Medical School, we learned that the Dreem was recently used in a study of fatigue in Qantas airline pilots. However, this system requires a connection to the internet in order to download and process the data. The Dreem does have enough onboard memory to store a person’s EEGs taken during sleep over 21 days. However, we did not want to wait until the end of our voyage in order to be able to confirm that we recorded valid data.
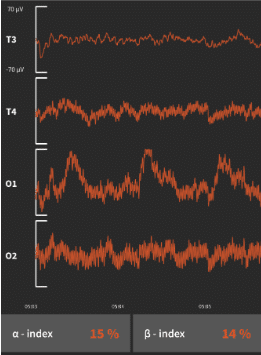
The BrainBit was inexpensive enough that we just bought a device and the recording software to see what we could get. Surprisingly, we were able to get reasonable readings during sleep from this 4-electrode device which records EEGs from both temporal lobes and both occipital (back of the head) lobes using a headband-like configuration. Furthermore, we were able to process these data in a software package called MATLAB using “multitaper spectrum analysis” to identify different sleep stages. Stay tuned for the next blog post to learn about the interim results of our study.

This is certainly interesting and going to be amazing. Good luck with it.
Exciting !
So you have a way to measure the boat movement? The waves and the boat movements may affect your sleep (positively) – check paper on sleep in rocking chair.
Thanks for the tip – can you send the link to the paper and we’ll check it out when we’re back on shore?
L’s EEG was always individual electrodes cemented to her head and then wrapped up like a mummy. They itched terribly. She seemed to be sensitive to the substance they used to hold them on. I like the one Greg is in. It looks more comfortable than what she had.
Nice write up on cleverly designed experiment. I’ll be interested in reactions as to whether the boat’s motion aids or detracts from sound sleep. The skipper knows I am to get a real exam on shore but think I would do better with some simulated ocean roll.
We’re trying to get a helicopter pad installed on Ingwe so you can test your hypothesis. The captain is sending good vibes to you.